Still, the disorder often has serious impacts on emotional, physical, and mental health. It can even be deadly if left untreated, so if you or a loved one are struggling, it’s important to find appropriate care.
What is Bulimia Nervosa? A Medical Definition
Like all eating disorders, bulimia nervosa is a mental illness that manifests as certain disordered eating behaviors. Specifically, bulimia nervosa involves periods of binge eating, followed by compensatory behavior, used to “make up” for the binges.
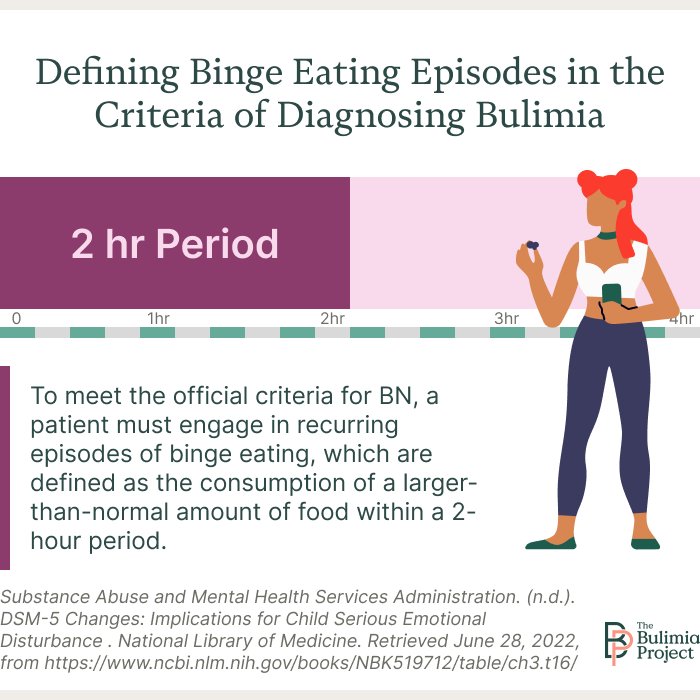
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), the official register of all recognized mental health disorders, a binge eating episode involves:1
- Eating an objectively large amount of food in a certain time period (usually two hours)
- A loss of control over what or how much food is consumed
With BN, these binging episodes are followed by compensatory purging behavior. Self-induced vomiting is a well-known purging method, but people struggling with bulimia may also:1
- Misuse or abuse of laxatives or diuretics
- Fast
- Exercise excessively
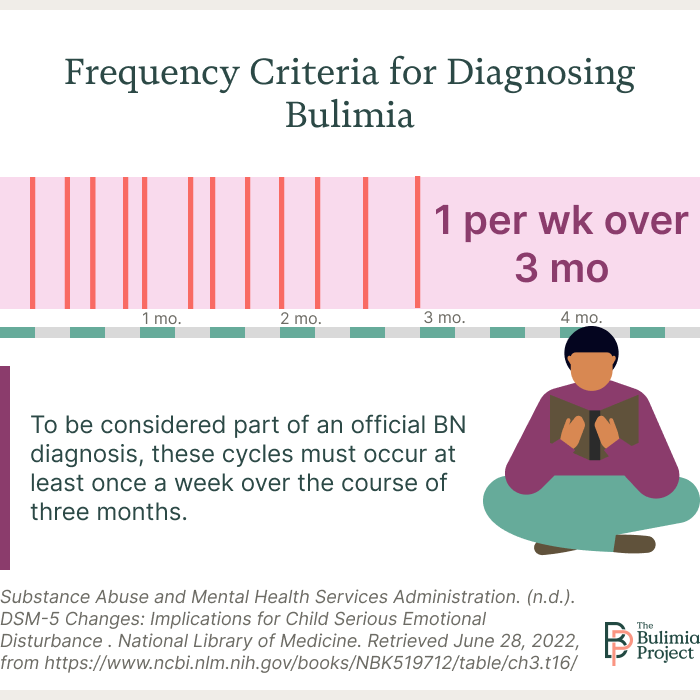
To medically diagnose bulimia nervosa, these behaviors must occur on average at least once a week for three consecutive months.1
What Causes Bulimia Nervosa?
As with other eating disorders, there is no one cause of bulimia nervosa. The behaviors involved are maladaptive coping mechanisms, and they develop and are triggered through a number of interlocking biological, psychological, and environmental factors.
Biological Factors
Although eating disorders such as BN and anorexia nervosa (AN) were once thought to be primarily socially driven, ongoing research has uncovered a number of biological factors that play a role in the development of these conditions.
Hormone dysregulation and hormonal changes, particularly those involved with puberty, have been linked to the onset of bulimia nervosa.2 Some people may have altered structures in their brain’s “reward center,” making it easier to develop binge eating behaviors.3 Overall, bulimia nervosa has been found to be moderately hereditary, meaning the condition can be genetically passed down.4
Psychological Factors
Several psychological factors can also influence the likelihood of someone developing an eating disorder like bulimia nervosa.
Many people who struggle with BN struggle with co-occurring mental health issues, including depression, anxiety, bipolar disorder, post-traumatic stress disorder, and panic disorder.5 And aside from being born with a predisposition to develop the disorder, people can also be born with certain traits—such as the way they handle stress—that make them more likely to exhibit binging and purging behaviors.4
Environmental Factors
Environmental factors also have a significant impact on the development or maintenance of bulimia nervosa.Sadly, BN has a very high overlap with experiencing trauma, especially trauma experienced early in life.6 Disordered eating behaviors, such as frequent dieting and compulsive exercise, along with body dissatisfaction and the tendency to equate appearance with self-worth, can also be modeled by parents and peers.7
Bulimia Nervosa Signs and Symptoms
When people ask, “What is bulimia?” many of them are likely thinking about how to identify the condition in themselves or someone else. There are many common signs and symptoms of bulimia nervosa, including:8
- A preoccupation with body shape, weight, or size
- Low self-esteem and/or high concern with appearance
- Frequently dieting or participating in fad diets
- Frequently visiting the bathroom shortly after eating
- Social isolation or secretive behavior
- Fear of, discomfort with, or avoiding eating around others
- Extreme or frequent mood swings
- Stealing, hiding, or hoarding food
- Excessive use of mouthwash, mints, or gum
Bulimia nervosa also manifests in a number of physical ways, such as:8
- Stomach cramps, acid reflux, and other gastrointestinal issues
- Constipation
- Dizziness
- Sleep disturbances
- Frequent sore throat
- Dental problems, such as cavities or enamel erosion
- Yellow or dry skin and brittle nails
- Menstrual irregularities
Although the desire to lose weight and the fear of gaining weight are common aspects of BN, many people with bulimia present at a normal weight or in larger bodies, which can make it harder to see the truth of the matter.8 It’s also possible for someone to struggle with BN without presenting any of these common indicators.
If you’re concerned a loved one is struggling with bulimia nervosa, the best way to approach the subject may be thoughtfully and lovingly asking them about it and listening with an open mind and heart.
Treating Bulimia Nervosa
Eating disorders are complex conditions impacting mental, physical, and emotional well-being. Generally, a multifaceted approach is needed to address these various concerns. Thankfully, there are a number of effective ways to treat bulimia nervosa.
Several types of psychotherapy—or talk therapy—have been found particularly helpful. Cognitive behavioral therapy (CBT) is the leading treatment for BN, helping patients recognize and better understand their unhelpful thought and behavioral patterns and offering them tools to avoid those triggers and develop healthier coping mechanisms.9
Interpersonal psychotherapy (IPT), where patients learn strategies to manage their personal relationships better, and dialectical behavior therapy (DBT), which focuses on skills like distress tolerance, mindfulness, and emotional regulation, have also been found to help.9
Many eating disorder patients also find help in “alternative” therapies or those that have not been as widely scientifically tested. People with BN have reported success with methods like light therapy, relaxation therapy, and acupuncture, though these were used as “complementary” therapies alongside more traditional psychotherapy approaches.10
Within Health offers a convenient, private, and specialized eating disorder recovery app
Our program provides IOP and PHP therapy options, meal kit deliveries, a remote-monitored numberless scale, and much more.
Call for a free consultation
Finding Help for Bulimia Nervosa
As there are many ways to treat bulimia nervosa, there are many avenues to find help for this condition.
You can start by speaking with a therapist, psychiatrist, or primary care physician. These experts can diagnose the condition, which opens the doors to many treatment programs or otherwise point you in the best direction for appropriate care. A number of websites and hotlines offer additional resources and information for those looking to get started.
Still, regardless of where you look for help, what matters most is looking. It’s the first step toward proactively creating a healthier and happier future.
Resources
- DSM-IV to DSM-5 Bulimia Nervosa Comparison. (2016). Substance Abuse and Mental Health Services Administration. Accessed February 2025.
- Baker JH, Girdler SS, Bulik CM. (2012). The role of reproductive hormones in the development and maintenance of eating disorders. Expert Review of Obstetrics & Gynecology; 7(6);573–583.
- Frank GK. (2013). Altered brain reward circuits in eating disorders: chicken or egg? Current Psychiatry Reports; 15(10);396.
- Berrettini W. (2004). The genetics of eating disorders. Psychiatry; 1(3):18–25.
- Woodside BD, Staab R. (2006). Management of Psychiatric Comorbidity in Anorexia Nervosa and Bulimia Nervosa. CNS Drugs; 20:655-663.
- Tagay S, Schlottbohm E, Reyes-Rodriguez ML, Repic N, Senf W. (2014). Eating disorders, trauma, PTSD, and psychosocial resources. Eating Disorders; 22(1):33–49.
- Mazzeo SE, Bulik CM. (2009). Environmental and genetic risk factors for eating disorders: what the clinician needs to know. Child and Adolescent Psychiatric Clinics of North America; 18(1):67–82.
- Bulimia Nervosa. (n.d.). National Eating Disorders Association.
- Murphy R, Straebler S, Cooper Z, Fairburn CG. (2010). Cognitive behavioral therapy for eating disorders. The Psychiatric Clinics of North America; 33(3):611–627.
- Fogarty S, Smith CA, Hay P. (2016). The role of complementary and alternative medicine in the treatment of eating disorders: A systematic review. Eating Behaviors; 21:179-188.