Here’s the good news: Bulimia is treatable, and most of the serious health problems associated with the disorder can be reversed. The key is to get treatment as early as possible. With ongoing care and support, you can effectively manage bulimia, helping you to embrace a healthy future.
Physical Bulimia Health Risks
Bulimia nervosa involves cycles of binge eating and purging through a variety of compensatory behaviors. Both of these aspects can take a heavy toll on the body.
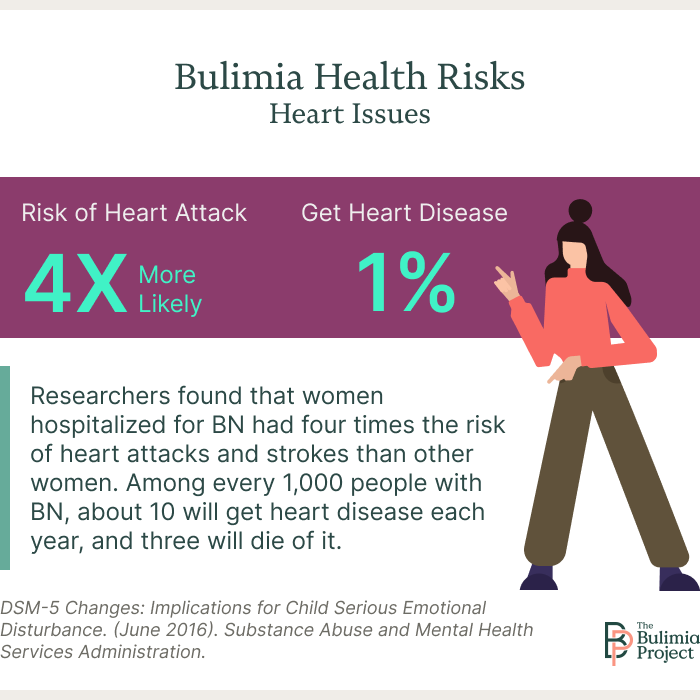
Heart Health
Bulimia nervosa is closely tied to several cardiovascular complications, including heart disease, arrhythmias, congestive heart failure, and sudden cardiac death.1 Primarily, these issues are tied to the electrolyte imbalances that often occur from purging, especially through self-induced vomiting, laxative misuse, or excessive exercise.1
In studies, researchers found that women hospitalized for BN had four times the risk of heart attacks and strokes than other women. Among every 1,000 people with BN, about 10 will get heart disease each year, and three will die of it.2
Digestive Issues
Digestive issues are among the most common medical complications of bulimia nervosa.
Heartburn and regurgitation issues are frequent, especially for people who utilize self-induced vomiting. Gastroesophageal reflux disease (GERD)—a form of chronic acid reflux—is also common.9Issues with swallowing can happen, once again, particularly for those who vomit as a compensatory behavior. Further damage to the esophagus is possible, including tears and Barrett’s disease. In severe cases, an increased risk of esophageal cancer has also been connected to bulimia nervosa.9
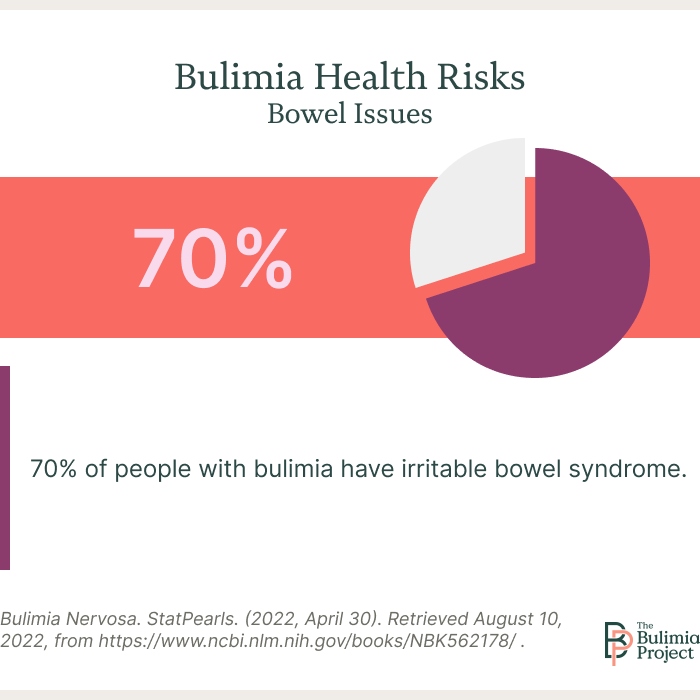
1. Bowels
Almost 70% of people with bulimia have irritable bowel syndrome. You may feel constipated for long stretches of time, and you may have several days during which you face relentless diarrhea.
Almost 70% of those suffering from bulimia have irritable bowel syndrome.
Bowel troubles can stem from electrolyte imbalances, but they can also begin with laxative abuse. Over-the-counter tools are meant for intermittent use.
Leaning on them repeatedly can cause such steep dehydration and damage that you can’t function without them. You’ll need a special diet and a bowel retraining program to get better.
2. Stomach
During a binge, some people eat so quickly that they feel bloated and are often in pain. Your stomach is meant to hold a small amount of food, but when you binge, you might take in an entire day’s worth of calories in one sitting. That feeling of fullness often entices people to purge.
Some people with longstanding bulimia feel pressure and nausea constantly, even when they’re not bingeing. You may also be unable to tell when you’re full after eating, as your stomach isn’t communicating with the brain properly.
3. Esophagus
Regular vomiting puts delicate throat tissues in contact with stomach acids. Repeated episodes can damage your esophagus and the tissues that keep your stomach closed. You might develop heartburn symptoms, and you might regurgitate food when you burp.
Some people develop esophageal tears from repeated vomiting. But many more develop longstanding throat and chest pain from esophagus burns.
Kidney Health
Electrolyte imbalances brought on by the disordered behaviors involved in BN can also lead to kidney health concerns. Chronic kidney disease and hypokalemic nephropathy, a health issue that can lead to a progressive loss of kidney function, are possible, particularly when the levels of phosphate, potassium, and magnesium are off.3
Oral Health
Purging through vomiting can significantly damage teeth, as the acids in vomit erode tooth enamel. This can result in tooth decay, gum disease, and damage to the salivary glands over time.5
If BN is treated and vomiting controlled, the effects of tooth decay and gum disease can be mitigated. But if teeth fall out, which can eventually happen, that damage is irreversible, and implants or other replacements are needed. Fillings or other dental repairs may also be required after a certain point.
Bone Health
The effects of laxative and diuretic misuse, self-induced vomiting, and disordered eating behaviors commonly presenting in BN often interfere with the ability to absorb nutrients properly. This can lead to several issues, including problems with bone health.
People with BN often have a calcium deficiency, resulting in brittle, weak bones.6 The condition has also been tied to lower bone density and a higher risk of osteoporosis.4
Mental Bulimia Health Risks
Bulimia nervosa is regarded as a mental health condition for a reason. The eating disorder can lead to several physical effects, but the behaviors are driven by unhelpful thoughts.
As with many other eating disorders, bulimia nervosa commonly co-occurs with other mental health disorders, including anxiety disorders and depression.10 It’s difficult, if not impossible, to determine whether anxiety and/or depression drives BN-related behavior or vice versa. Still, in any case, the co-occurrence can result in many additional mental health concerns, including a tendency to self-isolate, fear of eating around others, and chronically low self-esteem.11
Sadly, the mental health risks of bulimia nervosa can be deadly if left untreated. Suicide attempts among people with BN have been found to be frequent, and many patients attempt suicide multiple times. By one study’s count, nearly 28% of participants with BN had attempted suicide at least once.7
Emotional Bulimia Health Risks
The emotional health risks associated with bulimia nervosa tie in closely to bulimia health risks on mental well-being. On top of leading to self-isolation and other unhelpful experiences, BN has also been tied to:11
- Mood swings
- Frequent checking in the mirror (or avoiding the mirror)
- Sense of self-worth tied to appearance
- Frequent comparison between oneself and others, generally in a negative light
- Feelings of shame, guilt, and despair connected to eating behaviors
- Rigid rules or schedules around eating, which cause disturbance when not met
In many ways, the struggle with BN can become the center of someone’s world, and fixating on the problem or the negative feelings associated with it can do real harm to someone’s mental and emotional health.
Finding Help for Bulimia Nervosa
Bulimia nervosa is a serious eating disorder. If you or a loved one are experiencing bulimia health risks or other issues related to the disorder, it’s essential to seek out help.
With appropriate treatment, it’s possible to address the bulimia symptoms on your emotional, physical, and mental health. Depending on the severity of your case, your medical history, and other factors, there are several treatment avenues you can pursue.
Hospitalization
Eating disorders of all kinds are generally treated through psychotherapy and nutrition education. But sometimes, more extreme steps are needed.
If you’re dealing with severe nutritional deficiencies or mental health issues related to BN, an initial period of hospitalization may be recommended. This allows doctors to have round-the-clock supervision and give the care needed to address any immediate threats to someone’s life.
Inpatient hospitalization for eating disorders usually only lasts a few weeks. Once someone is considered medically stable, they can move on to other types of care, like residential treatment, which focuses on physical and mental health and institute long-term goals.
Therapy
Psychotherapy—or talk therapy—is the cornerstone of eating disorder treatment. Many types of therapy can help someone with an eating disorder. However, people struggling with BN tend to respond well to cognitive behavioral therapy (CBT), which works to help change both thoughts and behaviors.8
Therapy can be offered on an individual basis or in group sessions. Throughout the treatment process, someone may attend both types of therapy. Support groups, while not a specific type of “therapy,” per se, are also frequently considered therapeutic experiences. They offer a forum for people with BN to connect with others going through similar situations, discuss their concerns, and celebrate their successes, among other benefits.
Additional Support
Building a support network is one of the most essential aspects of lasting recovery. This can include members of your treatment team, family members, close friends, or anyone you feel you can consistently rely on and comfortably discuss difficult feelings with.
A support network can help increase your sense of accountability toward your recovery. It can make you feel like you’re part of something bigger than yourself and give you an outlet to share the burden or celebrate the wins along the way.
If you’re not enrolled in treatment, it’s time to get started. With a comprehensive treatment program, you can address issues that are contributing to your bulimia and begin to build a new life in recovery.
Resources
- Tith RM, Paradis G, Potter BJ, Low N, Healy-Profitós J, He S, Auger N. (2020). Association of Bulimia Nervosa With Long-term Risk of Cardiovascular Disease and Mortality Among Women. JAMA Psychiatry; 77(1):44–51.
- Rapaport L. (2019, October 22). Bulimia Tied to Higher Risk of Heart Disease and Premature Death. Reuters. Accessed March 2024.
- Puckett L. (2023). Renal and electrolyte complications in eating disorders: a comprehensive review. Journal of Eating Disorders; 11(1):26.
- Newton JR, Freeman CP, Hannan WJ, Cowen S. (1993). Osteoporosis and normal weight bulimia nervosa–which patients are at risk? Journal of Psychosomatic Research; 37(3):239–247.
- Hermont AP, Oliveira PA, Martins CC, Paiva SM, Pordeus IA, Auad SM. (2014). Tooth erosion and eating disorders: a systematic review and meta-analysis. PloS one; 9(11):e111123.
- Sagar A. (2005). Long Term Health Risks Due to Impaired Nutrition in Women with a Past History of Bulimia Nervosa. Nutrition Noteworthy; 7(1).
- Corcos M, Benoit-Lamy T, Paterniti S, Flament JMF. (2002). Suicide attempts in women with bulimia nervosa: frequency and characteristics. Acta Psychiatrica Scandanavica; 106(5):381-386.
- Murphy R, Straebler S, Cooper Z, Fairburn CG. (2010). Cognitive behavioral therapy for eating disorders. The Psychiatric Clinics of North America, 33(3):611–627.
- Santonicola A, Gagliardi M, Guarino MPL, Siniscalchi M, Ciacci C, Iovino, P. (2019). Eating Disorders and Gastrointestinal Diseases. Nutrients; 11(12):3038.
- Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H, Hofmeier S, Levine M, Crosby RD, Peat C, Runfola CD, Zimmer B, Moesner M, Marcus MD, Bulik CM. (2017). The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. Journal of Abnormal Psychology; 126(3):340–354.
- Bulimia Nervosa. (n.d.) National Eating Disorders Association. Accessed March 2024.